How to Improve PDC Scores: The Complete 2025 Guide
Key Takeaways
• The Stakes Have Never Been Higher: Medication non-adherence is an escalating crisis. As of 2025, 42% of patients alter their medication habits due to cost. This directly impacts your Proportion of Days Covered (PDC) scores.
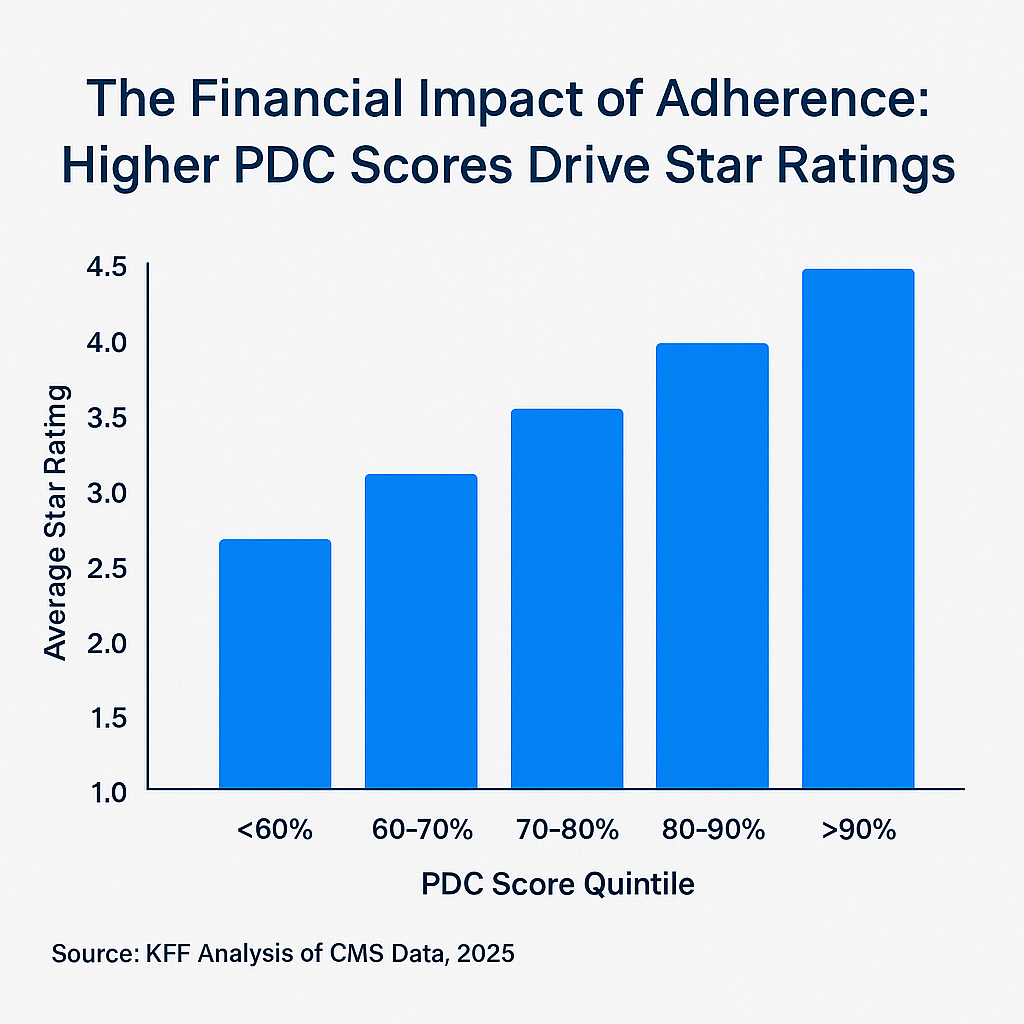
• PDC is a Financial Power Lever: With $12.7 billion in Medicare Advantage Quality Bonus Payments on the line, the triple-weighted PDC score is one of the most critical drivers of your plan's financial performance and stability.
• The Health Equity Index (HEI) Changes Everything: For the 2027 Star Ratings, the HEI makes improving adherence in vulnerable populations a direct, financially-incentivized mandate. The old playbook is no longer enough.
• The Proof is in the Data: Our platform demonstrates an 89% interaction completion rate with Medicare/Medicaid members, proving that empathetic, AI-driven conversation truly engages patients where other methods fail.
This exceptional engagement rate shows how the right approach transforms PDC improvement from a compliance burden into a patient success story.
Read 60-Day PDC Success Case StudyAs a leader in a health plan or provider organization, the pressure to improve medication adherence has never been greater. It's not just about the staggering cost of non-adherence. As of today, July 30, 2025, it's about two urgent, unavoidable realities: a worsening patient affordability crisis and a fundamental shift in how CMS measures performance.
Recent 2025 data shows that two-thirds of Americans now see their prescription costs as a financial burden. This isn't an abstract statistic; it's a driver of behavior. Simultaneously, with CMS's Health Equity Index (HEI) now a core component of future Star Ratings, your Proportion of Days Covered (PDC) score has become the focal point for both your financial health and your commitment to equitable care.
The old playbook—more call center agents, more generic text reminders—is fundamentally broken. It's a costly, low-impact approach that fails to build the operational resilience needed in this volatile landscape. At Rivvi, we believe it's time for a new playbook, one built not on broadcasting, but on understanding and evidence.
Explore how conversational AI infrastructure is delivering the evidence-based results health plans need in 2025.
Why PDC is More Than a Metric in 2025
At its core, the PDC formula is simple math. But in the high-stakes environment of Medicare Advantage, PDC is a triple-weighted measure and a powerful financial lever.
Quality Bonus Pool
PDC Weight Multiplier
Bad Contact Data
The real challenge isn't the math; it's discerning the signal from the noise. The "noise" is often more fundamental than you think. In a recent 90-day pilot with our first enterprise partner, a plan with 60,000 Medicare/Medicaid members, our platform immediately identified that 27% of the member contact numbers on file were disconnected or invalid.
Think about that. Over a quarter of their manual outreach efforts were guaranteed to fail before a single word was spoken. This is the foundational data problem that plagues adherence initiatives. The "signal," therefore, is not just knowing why a member is non-adherent, but first, having the ability to efficiently and systematically clean your data to even have the conversation.
Before you can solve for adherence, you have to solve for access. Our platform turns every interaction—and every failed interaction—into actionable intelligence that improves the efficiency of your entire operation.
The Core Flaw in the Old Adherence Playbook
The entire industry has spent years trying to solve adherence with one-way communication. We send texts, we make robocalls, we leave voicemails. We're broadcasting into a void, hoping something sticks.
Our entire company was built on a simple, powerful conviction: You can't fix a problem you don't understand.
You can't solve a financial barrier with a reminder text. You can't solve a transportation issue with a voicemail. This is the fundamental flaw in the old playbook. It assumes the problem is forgetfulness when the reality is infinitely more complex. For more on the inefficiencies of traditional methods, see our analysis on The Hidden Cost of Manual Medication Adherence Calls.
A Modern Playbook, Proven in the Real World
A modern adherence strategy must be designed to uncover and resolve the true barriers to care. It requires a shift from passive alerts to proactive, two-way conversations that actually engage members.
This isn't a theoretical ideal. In our enterprise pilot, our platform achieved an 89% interaction completion rate. This is a critical metric. When our HIPAA-compliant AI connects with a complex Medicare/Medicaid member, they don't hang up. They engage. The conversation is so natural and valuable that they see it through to the end.
This is how you move from reminders to resolutions. This is how you uncover the true "why" behind non-adherence by pinpointing barriers like:
Financial Toxicity
'My copay was higher than I expected this month.' - Identified through conversation, not surveys.
Transportation Barriers
'I couldn't get a ride to the pharmacy.' - Real-time problem solving vs. generic reminders.
Health Literacy Gaps
'I wasn't sure if I was supposed to keep taking it.' - Education delivered at point of confusion.
This actionable intelligence allows your clinical teams to stop wasting time on generic outreach and focus their expertise on solving the actual problems your members are facing. This is a core principle we explore further in our guide, Turning Payer Spreadsheets Into Revenue.
From Insight to Impact: Our Enterprise Pilot
When you shift your focus from broadcasting to understanding, the results are immediate and tangible.
Pilot Population
Interaction Completion
Positive Conversions
Complex Cases Identified
In our pilot with a 60,000-member Medicare/Medicaid plan, we didn't just gather data; we drove action. Our platform successfully guided 67 members to a positive conversion—confirming a prescription pickup, scheduling a visit, or another critical health action.
More importantly, our AI intelligently identified 33 members with complex needs that required human intervention. These were not generic support requests; these were members with specific clinical questions or concerns about side effects. Our system automatically flagged these conversations and triaged them directly to the plan's care management team.
This is the playbook in action: Technology handles the scale, while human experts are freed up to focus on the high-acuity cases technology uncovers.
Traditional PDC Outreach
Traditional PDC Outreach
AI-Driven Conversation Platform
This is the power of moving from generic outreach to intelligent intervention, a topic we cover when comparing Voice AI vs. Call Centers for Medicare Outreach.
The Future of Adherence is Here
We believe we're just scratching the surface of what's possible when you combine empathetic conversation with powerful, responsible AI. The future of healthcare isn't about more data; it's about more understanding.
Our pilot results prove it's possible to achieve an 89% completion rate and drive meaningful health actions, even in the most challenging populations. It's about moving from one-size-fits-all systems to a hyper-personalized approach that treats each member as an individual.
If you're ready to stop guessing why your members are non-adherent and build a strategy that truly solves their needs, then let's have a real conversation.
Request Your 15-Minute Demo to See the New Playbook in Action
Discover how AI-driven conversations can transform your PDC scores and capture quality bonuses.
Content Upgrade
Download our free, one-page PDF: The PDC Improvement Checklist for Quality Leaders. This practical tool provides a scannable list of actionable strategies your team can implement today to start improving your PDC scores.
Get a PDC Improvement Plan
Talk to our team about actionable strategies to improve your PDC scores.